A five-stage framework for healthcare transformation
As we discussed in part one of this series, the experiences of patients and their Healthcare Professionals (HCPs) are inextricably linked, each affecting the other both positively and negatively. Despite this, healthcare systems today typically consider the patient experience and HCP experience separately, overlooking the critical synergy of this relationship and the impact one has on the other.
Moreover, patient and HCP expectations are continuously evolving, shaped by advancements in technology, shifting cultural norms, and individual experiences. To truly transform healthcare we need a holistic approach that recognises this interconnectedness, and develops strategies and initiatives that bridge both.
Patients frequently encounter long wait times, disjointed communication and a lack of empathy, whilst at the same time HCPs are stretched thin, managing complex caseloads, administrative demands and the emotional demand of their work. These challenges impact not just individual satisfaction but also the overall effectiveness of the healthcare system, leading to decreased patient engagement and increasing burnout among HCPs.
This brings us to the challenge: How do we implement a Customer Experience (CX) strategy that addresses the needs of both patients and HCPs while fostering a more cohesive, human-centered system?
We believe the answer lies in adopting a Human Centered Design (HCD) approach, which places the experiences of patients and HCPs at the core of every decision. HCD enables us to move beyond surface-level improvements, uncovering the root causes of challenges and designing intuitive, empathetic solutions that resonate on both personal and systemic levels. By bridging the gap between expectations and perceptions, HCD creates a foundation for meaningful alignment and collaboration across the healthcare ecosystem.
At the heart of this strategy is our Human Experience Factory that integrates HCD principles into a structured approach, and consists of five stages:
Acquire
Articulate
Align
Apply
Assess
Each of these stages is designed to capture and address the real experiences of patients and HCPs, ensuring that insights guide actionable, human-centered solutions.
This model transforms data into usable insights and then meaningful strategies, enabling healthcare systems to continuously learn, adapt, and improve. By focusing on the human connection at every stage, we can personalise care for patients, equip HCPs with the tools and support they need, and create a healthcare system that drives measurable change while fostering engagement and trust. Through this framework, we ensure that every experience contributes to a better system for all stakeholders.
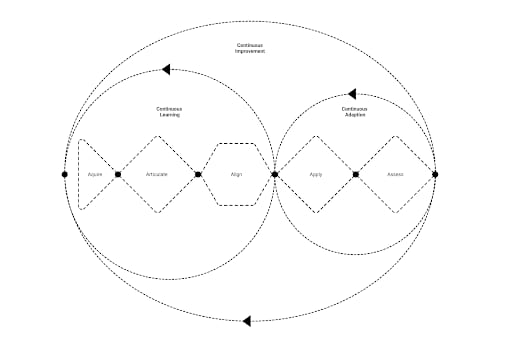
In this episode of our blog, we will explore how the first three stages of Acquire, Articulate, and Align form the foundation of the model’s continuous learning function.
Stage 1: Acquire
Start with data. Without it, we’re left guessing. Data helps us understand experiences, identify gaps, and measure progress. Whilst we regularly use data in our improvement and operational work, HCD derived data provides the additional richness of experiential content and context, and when combined with our established data and metrics offers an opportunity to truly understand the patient and HCP experience. Both quantitative and qualitative data play essential roles - quantitative data offers measurable metrics, while qualitative data reveals emotions, motivations, and daily realities. Viewing this through an HCD lens ensures we uncover the true needs and experiences of those at the heart of healthcare. Frameworks like the SERQUAL model provide structure, exploring dimensions like reliability, responsiveness, and empathy to shape actionable insights.
Experiential data bridges the gap between clinical, operational, and financial insights, capturing the emotional highs, friction points, and human connections that define care. Combined with other data types, it provides a holistic view that aligns with the Quadruple Aim: improving patient experience, enhancing provider well-being, reducing costs, and achieving better outcomes.
To gather meaningful insights, we must explore touchpoints across the healthcare ecosystem looking at multiple dimensions such as services, platforms, products, and interaction channels. Tools like PREMs, NPS, sentiment analysis, and HR surveys offer valuable perspectives but often present fragmented views, missing systemic issues affecting patients and HCPs.
Innovations like AI-driven mobile ethnography allow patients to document experiences in real-time, reducing recall bias and capturing richer insights. Personalising data collection with AI tailors questions to individual preferences, ensuring feedback is relevant and actionable. For instance, a patient facing long wait times might receive targeted questions about their visit, uncovering deeper insights to inform patient-centered solutions.
Experiential data, when integrated with clinical and operational insights, drives holistic transformation. By maintaining balance across the Quadruple Aim, we create systems that benefit patients, providers, and organisations, advancing the journey to value-based care.
HCD principles in practice
To ensure meaningful data collection, human-centered design principles guide how we engage with patients and HCPs:
Empathy starts with listening. By engaging in open-ended conversations, story telling and sharing, and meaningful dialogue, we create space for patients and HCPs to share their realities, uncovering emotional and practical insights. Asking an HCP to describe their day, for example, can highlight unseen challenges that impact their ability to provide care.
Understanding context is equally important. Observing care environments through shadowing HCPs or following patients as they navigate a hospital reveals barriers and inefficiencies that might otherwise go unnoticed. These observations help us see beyond what people say and into what they experience.
Collaboration is another key principle. Focus groups and workshops bring patients, HCPs, and stakeholders together, creating a platform for co-creation. These sessions uncover insights and ideas that reflect the lived realities of those at the heart of the system.
Finally, the process must be iterative. Feedback from initial findings can inform adjustments to surveys or focus group questions, allowing us to refine our approach and stay responsive to evolving needs.
- What if the key to improving healthcare outcomes lies not just in gathering data, but in how we listen, adapt, and act on the experiences of patients and HCPs in real-time?
Stage 2: Articulate
Once we’ve gathered the data, the next step is to articulate it by transforming raw information into meaningful insights that inspire action and guide change. This stage goes beyond simple analysis; it focuses on storytelling. A compelling narrative humanises data, connecting stakeholders to its purpose and aligning them around a shared vision for transformation. Storytelling bridges insights and action, laying the foundation for meaningful progress.
We begin by using tools like personas, journey maps, and service design blueprints to visualise the healthcare ecosystem. These tools map both the frontstage, where patients interact with care systems, and the backstage, where processes, people, and systems support these interactions. This dual perspective reveals "moments that matter," pivotal points where targeted interventions can drive the greatest impact for both patients and healthcare providers (HCPs).
While patients are the heroes of the healthcare journey, HCPs are the superheroes enabling it. Yet they are not alone; caregivers, communities, payors, administrators, health services, and pharmaceutical partners also play crucial roles. Articulating insights means weaving their contributions into the narrative, recognising the collaboration needed to drive holistic, system-wide change.
This stage is also where ideation begins. By presenting the “as-is” state, we empower teams to envision the “to-be” state. These discussions, grounded in data and real-world stories, spark creativity and innovation, uncovering bold solutions that reimagine patient and HCP experiences while considering the needs of the broader ecosystem.
Digital transformation plays a vital role here. Enhancing tools like patient portals, EHRs, and HCP dashboards or introducing new, innovative solutions creates seamless experiences across the ecosystem. Cross-functional collaboration ensures these digital interventions address specific needs, streamlining workflows for HCPs and personalising patient touchpoints to improve outcomes and satisfaction.
Emerging technologies like Generative AI and predictive analytics further enhance this stage. Predictive models help identify key "moments that matter," enabling stakeholders to prioritise interventions based on real-time and historical data. Generative AI synthesises insights into engaging narratives, bringing the "to-be" state to life and aligning teams on actionable, forward-thinking solutions.
Articulating insights connects people to the purpose of the work. By humanising data, visualising journeys, and telling the story of healthcare experiences, we foster collaboration and empower stakeholders to act. This stage ensures the path forward is not only clear and actionable but also deeply aligned with the needs of patients, HCPs, and the wider healthcare ecosystem.
HCD Principles in Practice
Visualisation for clarity: Tools like service design blueprints, journey maps, and personas turn data into visual representations, making the patient and HCP journey tangible. These tools bridge frontstage interactions and backstage systems, helping stakeholders connect the dots across people, processes, and tools.
Storytelling with data: Transforming complex data into relatable narratives highlights patterns, themes, and emotions. A compelling story ensures insights resonate, align stakeholders, and drive meaningful action.
Moments that matter: Prioritise the critical moments where trust is built or broken. These are the touchpoints that shape perceptions and offer the greatest potential for impactful change.
Validation and collaboration: Engage patients, HCPs, and support teams to validate insights and ensure solutions are grounded in reality. Co-creation fosters alignment, trust, and actionable outcomes.
What if understanding the moments that matter most could transform the way we deliver care?
Stage 3: Align
Once we’ve articulated insights from our data, the next step is to align, transforming ideas and opportunities into structured, prioritised actions that drive meaningful change. In healthcare, alignment is critical to bridge the gap between strategy and execution, ensuring that our vision translates into tangible improvements for both patients and healthcare providers (HCPs).
As the Chinese military general, strategist and philosopher Sun Tzu aptly said, “Strategy without tactics is the slowest route to victory. Tactics without strategy is the noise before defeat.” The Align phase connects the big picture with day-to-day realities, turning insights into impactful initiatives that resonate across the healthcare ecosystem.
Alignment in healthcare isn’t just about creating a plan; it’s about ensuring that every initiative reflects the lived experiences of those it impacts, both patients and HCPs. It requires balancing strategic objectives with the operational realities of care delivery, making sure that every action is practical, relevant, and focused on improving outcomes.
This phase is grounded in four interconnected stages - measure, frame, develop and map - that help translate insights into actions that drive progress while addressing the needs of all stakeholders in the healthcare system.
Measure
The first step in alignment is to measure, evaluating each opportunity against the realities of clinical settings, patient needs, and HCP constraints. This isn’t just about feasibility or cost; it’s about desirability and human impact. We ask questions like, “Will this solution reduce friction for HCPs? Will it meaningfully enhance the patient experience?”
In this stage, we assess technical feasibility, viability, and cost, alongside human factors like adoptability, learnability, and overall user impact. By balancing these considerations, we prioritise initiatives that address genuine pain points and have the potential to make a tangible difference in how care is delivered and experienced.
Frame
Once we’ve measured the opportunities, we move into frame, contextualising each initiative within the healthcare system’s unique operating model. This step ensures that each action aligns with the organisation’s strategic goals while remaining practical and impactful at the ground level. Frameworks like The Beryl Institute’s Experience Framework help us categorise initiatives across digital, cultural, and operational domains, ensuring they resonate with what both patients and HCPs need daily.
For example, framing might reveal that a digital improvement, such as enhancing the usability of patient portals, needs to be paired with a cultural initiative to foster empathy among care teams. By framing initiatives thoughtfully, we ensure that every opportunity supports broader goals while addressing specific, day-to-day challenges.
Develop
In develop, we transform the framed opportunities into actionable plans. This is where we define roles, allocate resources, and set timelines for implementation. Whether piloting a patient engagement tool, redesigning HCP workflows, or improving existing protocols, the focus is on creating clear, measurable pathways to change.
Cross-functional collaboration is key here. By involving diverse teams, clinicians, administrators, IT, and patient advocates, we ensure that plans are realistic and grounded in insights from all corners of the healthcare ecosystem. The goal is to craft solutions that are not only achievable but also considerate of the workload and expectations of both patients and HCPs.
Map
Finally, we map these initiatives to ensure alignment across teams and stakeholders. Mapping goes beyond organising logistics; it’s about building a shared commitment to improving patient and HCP experiences. This stage creates transparency by visualising how each initiative connects to the broader goals, showing every department and individual their role in the journey.
Mapping brings clarity to the process, helping teams see how their efforts contribute to a cohesive, human-centered system of care. Whether it’s patient-facing staff, clinical leads, or administrative teams, everyone can see how their contributions align with the shared vision of better outcomes and experiences.
Bringing it together
By aligning through measure, frame, develop, and map, we create a continuous thread that connects strategy to action. This structured approach ensures that every initiative is rooted in the realities of patient and HCP needs while supporting the broader goals of the healthcare system. Importantly, alignment helps us maintain balance in the system, ensuring that new processes, tools, or technologies enhance care delivery without adding unnecessary friction or complexity. It’s a thoughtful, deliberate process that keeps patient and HCP experience at the center of every decision, driving meaningful and sustainable transformation.
Continuous learning
By implementing the first three steps of the Human Experience Factory (Acquire, Articulate, and Align) you create a continuous learning cycle where insights inform actions, actions drive improvements, and improvements generate new insights. This iterative process ensures that strategies remain dynamic, relevant, and deeply connected to the evolving needs of patients, HCPs, and the broader healthcare ecosystem.
While we focus on this process from the perspective of care delivery and the organisations within it, its value lies in its holistic view. It allows us to ensure that every solution not only addresses immediate challenges but also makes sense within the broader healthcare ecosystem.
This approach helps us see the critical balance required when introducing interventions such as new processes, tools, or technologies. Each change must harmonise with the existing system to avoid unintended consequences and maintain equilibrium for both patients and healthcare providers. By embedding this thoughtful balance into every stage of the cycle, we create an adaptable, human-centered foundation that drives meaningful, sustainable improvements across the continuum of care.
While this first part of the journey has focused on how we gather and articulate insights, and align them with strategy, the next steps ‘Apply’ and ‘Assess’ are where those insights come to life in practical, measurable ways.
Are you currently working on a new innovation in healthcare? How might it influence the overall experience, and what steps can you take to ensure it maintains balance for both patients and HCPs?











